WE have a sense, a gut feeling if you like, that we know pain when it presents. We recognise distress when we see it – in people and in animals that we know well. We can’t always describe it in objective terms, but we recognise it. Sometimes it’s just in the ‘pained’ look in his or her eye or can be described by owners as ‘off-colour’ or ‘just not herself’ today.
In fact, some of these features can be captured in a scientific manner by measurements, such as the (animal) grimace scale. For the dog and horse, this features descriptions of how the lines round his muzzle and eyes tighten, how ear position varies with mood, changes in the set of his jaw.
Physical and mental
Pain comes in many forms, being variously described as acute or chronic, visceral or somatic, tractable or unremitting. Pain may arise from many sources, both physical and mental, and cause further illness, both physical and mental, in equines as for humans. We are all sentient beings, after all.
Behavioural change
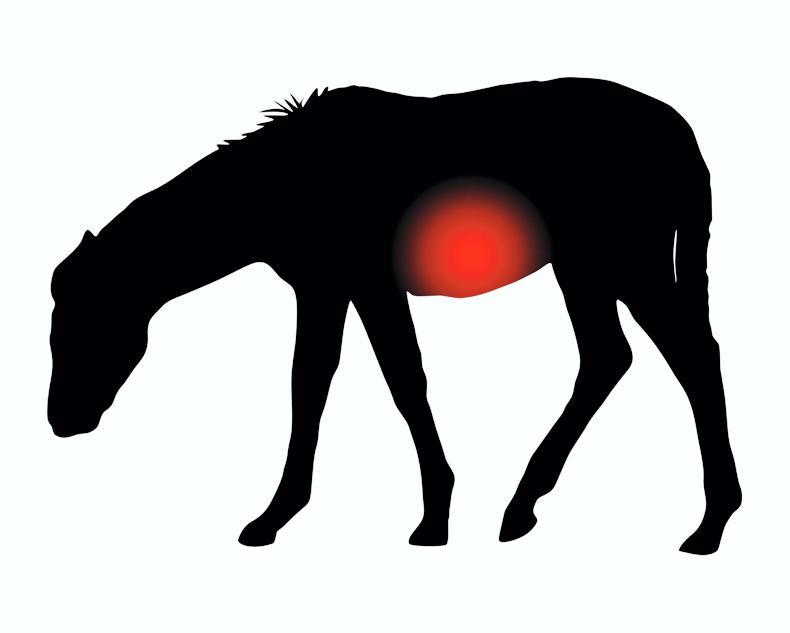
A horse in pain is seen by us to act differently in some way. Vets and owners are often taught to ‘know the normal; you will then better recognise the abnormal’. This behavioural change may be related to the source of pain. A lame horse will stand and move in an abnormal manner; a colicky horse may repeatedly get up and down, look or kick at his belly; teeth grinding, wood chewing and excessive salivation may indicate stomach pain – ulcers perhaps. Or the change may be more generalised in nature – a dull donkey with head held low, a social character standing isolated from the group, a pony refusing foods he normally wolfs down.
Head-nods and hip hikes
Veterinary science sometimes gives us quasi-objective scores, in particular in orthopaedics. We have long been used to grading the severity of lameness, usually on a scale of one to 10, watching horses walk and trot in straight lines and lunge in circles, sometimes varying the surface underfoot. We compare front and hind limb swing and stance phases, look for head-nods and hip hikes, compare ridden to in-hand gaits. Sometimes markers are placed on bony prominences and video-analysis conducted and there are now AI programmes utilised for gait analysis. Sometimes different riders are employed, some vets ride the animal themselves. But in other regards the art as well as the science are vital.
Hardy animals
Donkeys deserve special mention - as being different in the pain stakes. Not being as swift as horses, they have evolved to deal with adversity more by facing it than fleeing from it. They have more ‘fight than flight’ compared to horses and, in this model, showing pain and distress is to draw attention to oneself as weak, as a potential victim to a predator. Donkeys are more likely to mask the true extent of their suffering, sometimes fooling us into thinking they are less severely ill than they really are. We may dismiss them as ‘stoic’, but the dull donkey is a genuine veterinary emergency, worthy of proper investigation early, as otherwise it may prove to be too late.
Whether we can cure or even control pain depends of course on the specifics of its source, its severity, its cause and the nature of the patient themselves.
Relieve the pain
Drugs are one possible answer, addressing pain at pain receptors locally, at nerve fibres carrying pain signals or indeed at the perception of pain centrally – the brain itself. We have increasingly powerful analgesics (pain-relieving drugs). Many of these are anti-inflammatory in addition – the so-called NSAIDs (non-steroidal anti-inflammatory drugs) – they don’t simply relieve the pain, but they also dampen down the inflammatory process that is often the root cause.
Readers may be familiar with taking aspirin tablets, paracetamol, which acts centrally, or applying ibuprofen gel locally to inflamed parts. So the pain of fetlock arthritis or flexor tendonitis can be relieved using phenylbutazone, flunixin or other drugs from the NSAID family – by injection or as powder/paste orally. These drugs also (to varying degrees) have the ability to influence blood clotting and reduce fever and endotoxic shock, and are sometimes used with these properties primarily in mind. Indeed, we sometimes use pure anti-inflammatory agents (the corticosteroids) to reduce inflammation; this has the secondary effect of reducing pain too; and such agents are commonly injected into horses’ joints.
We have local anaesthetics to block the transmission of pain signals along nerves; and general anaesthetics to remove one’s ability to appreciate pain at all. We have ‘pure’ analgesic agents too, ones typically belonging to the opioid class, which act to remove the animal’s awareness of the pain or distress they have been feeling.
Misuse
These drugs commonly have a sedative effect also and are listed as ‘controlled drugs’ in misuse of drugs legislation, due to their potential harmful effects in humans. A few issues arise that are worth further mention: some of these drugs, e.g. bute, do not have a meat withdrawal period and must only be used in equines permanently (by way of their passport) excluded from the food chain. Some of these drugs, e.g. flunixin, can mask serious underlying disease, such as a surgical colic, thereby delaying referral and correct decision-making, with sometimes fatal results.
We need to balance therapy and welfare carefully, so that we don’t ask horses to compete when they would be otherwise unfit. We need to steer clear of accusations of doping (cheating) in performance horses – so that drug administration doesn’t lead to a positive doping finding, either through an inadvertent failure to observe drug clearance times, or intentionally malice.
Other ways
But drugs aren’t everything in this conversation: we can relieve pain in other ways too. Readers will be familiar with applying support bandages to an injured part, such as a forelimb tendon; applying splints and casts to fractured bones; tethering or box-resting a horse with a damaged pelvis. These all aim, in their own way, to reduce unnecessary movement of an injured part, thereby stopping those nerves from firing off the signals of pain.
We might influence these signals too with acupuncture, using laser or needles to align energy channels or potentially release endorphins – those natural substances that give us the ‘high’ of strenuous exercise.
Sometimes a change in environment, diet and/or management is in order, as part of the management of stress-induced gastric ulceration for example. Cold is another powerful and useful analgesic (as well as anti-inflammatory) – which of us hasn’t spent hours icing and cold-hosing horses’ legs after their and our athletic efforts? Rugby players don’t get into ice-baths for the fun of it!
A CAVEAT here: pain can be protective – nature’s way of stopping us from continuing to move the damaged part and damaging it further – so we need to be careful. The principle is most urgently in play when a fallen rider, with any possibility of spinal damage, is urged to remain immobile until professionally assessed. As a corollary, a horse on a controlled exercise programme shouldn’t be tacked up and ridden over a line of fences, just because you are feeling in the mood for a jolly. We have to face the reality that not all pain and distress, or the disease processes causing these, can be managed medically.
Sometimes the cause of colic, a twisted bowel perhaps, requires surgical correction; some fractures need surgical fixation with plates and screws; and some causes cannot reasonably be rectified at all. The horse that fractures at racing speed often has so much more tissue damage than the broken bone itself; the animal’s temperament may not accommodate the prolonged and arduous road to recovery ahead; the owner’s pocket may simply not be deep enough for the journey. Vets see ponies in overturned vehicles on the motorway, horses stuck in ditches and with limbs through holes in lorry ramps, partitions and floors. But the most upsetting pain-stories often have not been these horrific incidents, so long as they lead to a swift resolution. Instead they’ve been the horses we have battled to save over long periods, such as nursing a pregnant broodmare with chronic laminitis to term, knowing a foster mare would be needed or watching the pony they operated on for hours break a leg badly trying to stand up afterwards, knowing there was only one course of action left open.
Euthanasia is an emotive subject, for vets as well as for the owners of horses, one not to be dismissed lightly or spoken of frivolously. It can be the ultimate veterinary privilege not just to cure, but sometimes to end intractable pain in an animal that has suffered severely or at length with no further prospect of relief.



 This is a subscriber-only article
This is a subscriber-only article
 It looks like you're browsing in private mode
It looks like you're browsing in private mode






SHARING OPTIONS: